Endogenous Pursuit of Peace: Care about Your Microbiota
TRANSCEND MEMBERS, 17 Mar 2025
Prof Hoosen Vawda – TRANSCEND Media Service
You Will Achieve Peace and Your Body Will Last Longer
***********************
You are strongly urged to read this if you wish to enjoy peace and excellence in sustained health, irrespective of age. Parental guidance is recommended for minors, who may use this publication as a project, resource material.
***********************

A satirical cartoon: The Microbiota and its effect on the body. Note the elements in the graphic.
Photo credit: Specially commissioned satirical graphic by Chat GPT, for sole use in this publication, as a service to Transcend Peace Journalism.
The Human Microbiome: A new frontier in health [1]
This publication discusses the human microbiome, which in reality is another essential organ, analogous to any other organ in the body, such as the liver, kidneys, lungs, which is larger than any other body part, it is made up of trillions of microorganisms, which silently[2]functions in maintain a healthy body state. This organ is an essential body component, for the wellbeing and survival of humans. This is the human microbiota, which has been identified in the past five years, as an entity, responsible not only for sustained excellence in physical health, but also mental wellbeing and endogenous peace, within.
Gut microbiota, gut microbiome, or gut flora
These are the microorganisms, including bacteria, archaea, fungi, and viruses, that live in the digestive tracts of animals.[3],[4]. The gastrointestinal metagenome is the aggregate of all the genomes of the gut microbiota.[5],[6]. The gut is the main location of the human microbiome.[7] The gut microbiota has broad impacts, including effects on colonization, resistance to pathogens, maintaining the intestinal epithelium, metabolizing dietary and pharmaceutical compounds, controlling immune function, and even behavior through the gut–brain axis.[8]
The Gastric microbiota refers to the community of microorganisms, including bacteria, viruses, fungi, and other microbes, that reside in the stomach. While the stomach was once thought to be a largely sterile environment due to its acidic conditions, recent research has revealed that it hosts a diverse and dynamic microbial community. This community plays a crucial role in maintaining gastric health and overall well-being. Below is a comprehensive overview of gastric microbiota:
- Overview of Gastric Microbiota
- Definition: Gastric microbiota consists of the microorganisms that inhabit the stomach. It is part of the larger human microbiome, which includes microbial communities in the gut, skin, mouth, and other body sites.
- Diversity: The stomach’s acidic environment (pH ~1.5-3.5) limits microbial diversity compared to other parts of the gastrointestinal (GI) tract, but it still harbors a unique set of microbes adapted to these conditions.
- Key Players: The most common bacterial phyla in the stomach include Proteobacteria, Firmicutes, Bacteroidetes, Actinobacteria, and Fusobacteria. The most well-known gastric bacterium is Helicobacter pylori, which has significant implications for gastric health.
- Factors Influencing Gastric Microbiota
The composition of gastric microbiota is influenced by several factors:
- Gastric Acidity: The low pH of the stomach acts as a barrier to many microbes, but some, like H. pylori, have evolved mechanisms to survive.
- Diet: Food intake affects the microbial community by altering the stomach’s pH and providing nutrients for specific microbes.
- Medications: Proton pump inhibitors (PPIs), antibiotics, and other drugs can disrupt the balance of gastric microbiota.
- Age: Microbial composition changes with age, influenced by factors like diet, immune function, and exposure to pathogens.
- Disease States: Conditions like gastritis, peptic ulcers, and gastric cancer can alter the microbial community.
- Lifestyle: Smoking, alcohol consumption, and stress can also impact gastric microbiota.
- Role of Helicobacter pylori
- H. pylori is a Gram-negative bacterium that colonizes the stomach lining and is present in about 50% of the global population.
- Positive Roles: It may play a role in regulating immune function and protecting against certain diseases, such as asthma and gastroesophageal reflux disease (GERD).
- Negative Roles: It is a major risk factor for gastritis, peptic ulcers, and gastric cancer. Chronic infection with H. pylori can lead to inflammation and damage to the gastric mucosa.
- Adaptation: H. pylori produces urease, an enzyme that neutralizes stomach acid, allowing it to survive in the harsh gastric environment.
- Functions of Gastric Microbiota
The gastric microbiota contributes to several physiological processes:
- Barrier Function: It helps maintain the integrity of the gastric lining and prevents colonization by pathogens.
- Immune Modulation: It interacts with the immune system to regulate responses to pathogens and maintain tolerance to commensal microbes.
- Metabolic Activities: Gastric microbes participate in the breakdown of dietary components and the production of metabolites like short-chain fatty acids (SCFAs).
- Protection Against Disease: A balanced gastric microbiota can protect against infections and inflammatory conditions.
- Dysbiosis and Disease
Dysbiosis, or an imbalance in the gastric microbiota, is associated with various gastric and systemic diseases:
- Gastritis and Peptic Ulcers: Often linked to H. pylori infection, but other microbes may also play a role.
- Gastric Cancer: Chronic inflammation caused by H. pylori and dysbiosis can lead to gastric adenocarcinoma.
- GERD and Barrett’s Oesophagus: Alterations in gastric microbiota may contribute to these conditions.
- Obesity and Metabolic Disorders: Emerging evidence suggests a link between gastric microbiota and systemic metabolic health.
- Research and Therapeutic Implications
- Microbiome Analysis: Advances in sequencing technologies (e.g., 16S rRNA sequencing) have enabled detailed studies of gastric microbiota composition and function.
- Probiotics and Prebiotics: These are being explored as tools to restore a healthy gastric microbiota and treat conditions like H. pylori infection.
- Faecal Microbiota Transplantation (FMT): While primarily used for gut disorders, FMT is being investigated for its potential to modulate gastric microbiota.
- Targeted Therapies: Researchers are developing strategies to selectively target harmful microbes (e.g., H. pylori) while preserving beneficial ones.
- Future Directions
- Personalized Medicine: Understanding individual variations in gastric microbiota could lead to tailored treatments for gastric diseases.
- Microbiome-Based Diagnostics: Gastric microbiota profiles may serve as biomarkers for early detection of diseases like gastric cancer.
- Functional Studies: Further research is needed to elucidate the specific roles of different microbes and their interactions with the host.
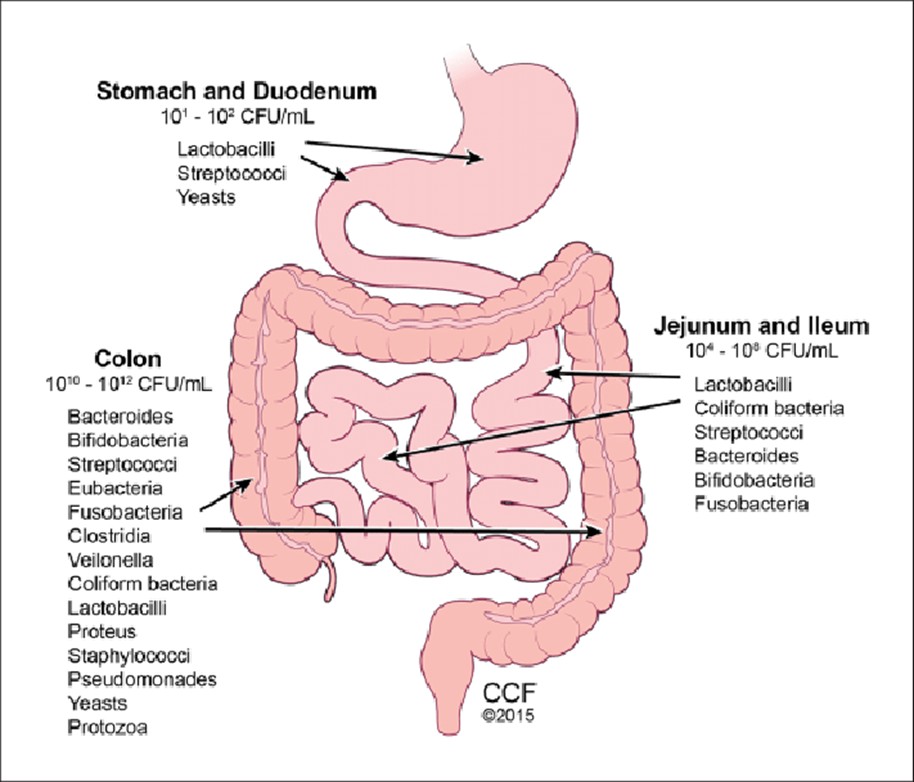
The human gut microbiota. Illustration by David Schumick, BS, CMI. Reprinted with the permission of the Cleveland Clinic Center for Medical Art & Photography © 2015. All rights reserved. CCF, Cleveland Clinic Foundation; CFU, colony-forming units.
- Gastric Microbiota and Obesity: Overview
- Microbiota-Host Interaction: The gastric microbiota interacts with the host’s metabolism, immune system, and hormonal regulation, influencing energy balance and fat storage.
- Dysbiosis and Obesity: An imbalance in the gastric and gut microbiota (dysbiosis) is associated with metabolic disorders, including obesity. Dysbiosis can lead to increased energy harvest from food, inflammation, and insulin resistance, all of which contribute to fat accumulation, particularly in the abdominal region.
- Mechanisms Linking Gastric Microbiota to Truncal Obesity
Several mechanisms explain how gastric microbiota may contribute to truncal obesity:
- Energy Harvest and Metabolism
-
- Gastric and gut microbes break down complex carbohydrates and fibers that the host cannot digest, producing short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate.
- While SCFAs have beneficial effects, an overabundance can lead to increased calorie absorption and fat storage, particularly in visceral adipose tissue (fat around the abdomen).
- Inflammation and Insulin Resistance
-
- Dysbiosis can trigger low-grade chronic inflammation by increasing the permeability of the gastric and intestinal lining (leaky gut), allowing bacterial endotoxins like lipopolysaccharide (LPS) to enter the bloodstream.
- This systemic inflammation promotes insulin resistance, a key driver of truncal obesity, as it leads to elevated insulin levels and increased fat storage in the abdominal region.
- Hormonal Regulation
-
- Gastric microbiota influences the production of hormones like ghrelin (the “hunger hormone”) and leptin (the “satiety hormone”), which regulate appetite and energy balance.
- Dysbiosis can disrupt these hormones, leading to overeating and weight gain, particularly in the trunk.
- Bile Acid Metabolism
-
- Microbes in the stomach and gut modify bile acids, which play a role in fat digestion and metabolic regulation.
- Altered bile acid metabolism due to dysbiosis can impair fat breakdown and contribute to obesity.
- Role of Helicobacter pylori[9]
-
- H. pylori infection has been linked to both weight loss and weight gain, depending on the stage and severity of infection.
- Chronic H. pylori infection may alter gastric hormones like ghrelin, leading to increased appetite and fat accumulation.
- Abnormal Lifestyle Factors and Their Impact on Gastric Microbiota
Abnormal lifestyle choices can disrupt gastric microbiota, contributing to truncal obesity:
- Poor Diet
- High-Fat, High-Sugar Diets: These diets promote the growth of harmful bacteria and reduce microbial diversity, leading to dysbiosis.
- Low Fiber Intake: Fiber is essential for feeding beneficial bacteria. A lack of fiber can reduce SCFA production and impair metabolic health.
- Physical Inactivity
- Sedentary behaviour is associated with reduced microbial diversity and increased inflammation, both of which are linked to obesity.
- Chronic Stress
- Stress alters the composition of gastric and gut microbiota, promoting the growth of inflammation-inducing bacteria and reducing beneficial microbes.
- Stress also increases cortisol levels, which promotes fat storage in the abdominal area.
- Poor sleep quality and duration can disrupt the circadian rhythm of gastric and gut microbiota, leading to metabolic imbalances and weight gain.
- Alcohol and Smoking [12]
- Excessive alcohol consumption and smoking can damage the gastric lining and alter microbial composition, contributing to dysbiosis and obesity.
- Human Studies: Gastric bypass surgery alters the microbiome, hence weight loss. Specific research has shown that individuals with truncal obesity often have altered gastric and gut microbiota compared to lean individuals. For example, they may have higher levels of Firmicutes and lower levels of Bacteroidetes.[15], [16] The Firmicutes/Bacteroidetes (F/B) ratio is a crucial indicator of gut health, influencing metabolism, immunity, and hormone regulation. Imbalances in the F/B ratio are associated with conditions like obesity, diabetes, cardiovascular diseases, autoimmune disorders, and mental health issues.
- Animal Studies: Experiments in mice have demonstrated that transplanting microbiota from obese individuals into germ-free mice leads to weight gain and fat accumulation, particularly in the abdominal region.
- Therapeutic Implications
Understanding the role of gastric microbiota in truncal obesity opens up new avenues for prevention and treatment:
- Dietary Interventions
- High-Fiber Diets: Promote the growth of beneficial bacteria and increase SCFA production.
- Probiotics and Prebiotics: These can help restore a healthy microbial balance and reduce inflammation.
- Lifestyle Modifications
- Regular Exercise: Physical activity enhances microbial diversity and reduces inflammation.
- Stress Management: Techniques like meditation and yoga can improve microbial health.
- Pharmacological Approaches
- Antibiotics: Targeted antibiotics may be used to treat dysbiosis, but their use must be carefully managed to avoid further disruption.
- Microbiota-Targeted Drugs: Emerging therapies aim to modulate specific microbial pathways involved in obesity.
- Faecal Microbiota Transplantation (FMT)[17]
- FMT, which involves transferring microbiota from a healthy donor, is being explored as a treatment for obesity and metabolic disorders.
- Future Directions
- Personalized Nutrition[18]: Tailoring diets based on individual microbiota profiles to prevent and treat obesity.
- Microbiome-Based Biomarkers[19]: Identifying microbial signatures associated with truncal obesity for early diagnosis and intervention.
- Functional Studies: Further research is needed to understand the specific roles of gastric microbes in obesity and metabolic health.
- Summary
Gastric microbiota plays a significant role in the development of acquired truncal obesity, particularly in the context of abnormal lifestyle factors. Dysbiosis in the gastric and gut microbiota can lead to increased energy harvest, inflammation, insulin resistance, and hormonal imbalances, all of which contribute to fat accumulation in the abdominal region. Addressing dysbiosis through dietary, lifestyle, and therapeutic interventions holds promise for preventing and treating truncal obesity. The author needs to clarify is that this microbiota called “Gastric” when it involves the entire gastrointestinal tract from the mouth to the anal orifice Is it a misnomer? This is a relevant question! The term “gastric microbiota” can indeed be a misleading if interpreted too broadly. This needs elucidation:
- What Does “Gastric” Refer To?
- The term “gastric” specifically refers to the stomach. It comes from the Greek word gaster, meaning stomach.
- Therefore, gastric microbiota strictly refers to the microbial community residing in the stomach, not the entire gastrointestinal (GI) tract.
- Microbiota Along the Gastrointestinal Tract
The GI tract is a long, continuous tube from the mouth to the anus, and each section has its own unique microbial community due to differences in pH, oxygen levels, nutrient availability, and other environmental factors. A healthy gut microbiome will ensure not only excellence in physical health, but also mental health with regards to cognition, behavioural pattern, mood swings and is in even implicated in the genesis of degenerative brain diseases, especially in the geriatric population.[20],[21]. It is important to note that gut microbiome plays a fundamental role in early brain development, as well.
- Oral Microbiota
- Located in the mouth.
- Includes bacteria, fungi, and viruses adapted to the oral environment.
- Plays a role in oral health and can influence downstream microbial communities.
- Gastric Microbiota
- Located in the stomach.
- Dominated by acid-tolerant microbes like Helicobacter pylori.
- Less diverse due to the highly acidic environment.
- Small Intestinal Microbiota
- Located in the small intestine (duodenum, jejunum, ileum).
- Relatively low microbial density compared to the colon.
- Involved in nutrient absorption and immune regulation.
- Colonic Microbiota
- Located in the large intestine (colon).
- The most dense and diverse microbial community in the GI tract.
- Plays a major role in fermenting undigested carbohydrates, producing short-chain fatty acids (SCFAs), and maintaining gut health.
- Rectal and Anal Microbiota
- Located in the rectum and anal orifice.
- Similar to colonic microbiota but may include additional microbes from the external environment.
- Is “Gastric Microbiota” a Misnomer?
- Yes, if used to describe the microbiota of the entire GI tract. The term “gastric” is specific to the stomach and should not be used interchangeably with terms like “gut microbiota” or “intestinal microbiota,” which refer to the microbial communities in the intestines.
- No, if used correctly to refer only to the microbial community in the stomach.
- Correct Terminology
- Gastric Microbiota: Refers only to the microbes in the stomach.
- Gut Microbiota: Refers to the microbes in the intestines (small and large intestines).
- Gastrointestinal Microbiota: Refers to the microbes throughout the entire GI tract, from the mouth to the anus.
- Oral Microbiota: Refers to the microbes in the mouth.
- Faecal Microbiota: Refers to the microbes in stool, which primarily represent the colonic microbiota.
- Why the Confusion?
- The term “gastric microbiota” is sometimes used loosely in popular science or non-specialist literature, leading to confusion.
- Additionally, the stomach is part of the GI tract, so people may mistakenly assume “gastric microbiota” refers to the entire tract.
- Importance of Precision
- Using precise terminology is crucial in scientific and medical contexts to avoid misunderstandings.
- For example, when discussing diseases like obesity, it is important to specify whether referring to gastric, intestinal, or overall GI microbiota, as their roles and mechanisms may differ.
- Conclusion
The term “gastric microbiota” is not a misnomer when used correctly to describe the microbial community in the stomach. However, it should not be used to refer to the microbiota of the entire gastrointestinal tract. For the broader microbial community, terms like “gut microbiota” or “gastrointestinal microbiota” are more appropriate.
A ground-breaking research was likely one of the seminal experiments in microbiome research that demonstrated the role of gut microbiota in obesity. While the term “gastric microbiota” is specific to the stomach, the study refers to and focused on gut microbiota (intestinal microbiota) and its impact on obesity. It is necessary to provide some context and details about this research and its implications for human obesity management.
- The Mouse Obesity Study
The study was conducted by Dr. Jeffrey Gordon and his team at Washington University in St. Louis. While their work primarily focused on the gut microbiota (intestinal microbiota), it revolutionized understanding of how microbes influence obesity. Here’s a summary of their findings:
- Experimental Design
- The researchers used germ-free mice (mice raised in sterile conditions with no microbiota).
- They transplanted gut microbiota from obese mice and lean mice into these germ-free mice.
- The mice were fed the same diet, and their weight and metabolism were monitored.
- Key Findings
- Mice that received microbiota from obese donors gained significantly more weight and fat mass compared to those that received microbiota from lean donors.
- The obese microbiota was more efficient at extracting energy from food, leading to increased calorie absorption and fat storage.
- The study demonstrated that gut microbiota plays a causal role in obesity, not just a correlative one.
- Mechanism
- The obese microbiota had a higher ratio of Firmicutes to Bacteroidetes, two major bacterial phyla in the gut.
- These microbes were better at breaking down complex carbohydrates and fibers, producing more short-chain fatty acids (SCFAs), which are absorbed by the host and contribute to energy harvest.
- Implications for Human Obesity
This study had profound implications for understanding and managing human obesity. Here’s how it has influenced research and treatment strategies:
- Microbiota as a Key Player in Obesity
- The study confirmed that gut microbiota is a major factor in energy balance and fat storage, independent of diet and genetics.
- It highlighted the importance of microbial diversity and composition in maintaining a healthy weight.
- Potential for Microbiota-Based Therapies
- Probiotics and Prebiotics: These are being explored as tools to modulate gut microbiota and promote weight loss.
- Faecal Microbiota Transplantation (FMT): Transplanting microbiota from lean donors to obese individuals is being investigated as a treatment for obesity and metabolic disorders.
- Dietary Interventions: High-fiber diets, fermented foods, and personalized nutrition plans are being developed to promote a healthy gut microbiota.
- Biomarkers for Obesity
- The ratio of Firmicutes to Bacteroidetes and other microbial signatures are being studied as potential biomarkers for obesity and metabolic health.
- Targeting Microbial Pathways
- Researchers are exploring ways to target specific microbial enzymes or metabolites involved in energy harvest and fat storage.
- Limitations and Challenges
While the study was ground-breaking, there are some limitations and challenges in translating these findings to humans:
- Complexity of Human Microbiota: Human microbiota is far more complex and variable than that of mice, making it harder to draw direct conclusions.
- Individual Variability: Factors like genetics, diet, lifestyle, and environment influence microbiota composition, making personalized approaches necessary.
- Causality vs. Correlation: While the study showed causality in mice, establishing causality in humans is more challenging.
- Current Research and Future Directions
Since the original study, research on the gut microbiota and obesity has expanded significantly. Here are some key areas of focus:
- Mechanistic Studies: Understanding how specific microbes and their metabolites influence host metabolism.
- Clinical Trials: Testing the efficacy of microbiota-based therapies like FMT, probiotics, and prebiotics in humans.
- Personalized Medicine: Developing microbiome-based diagnostics and treatments tailored to individual microbiota profiles.
- Lifestyle Interventions: Studying how diet, exercise, and stress management can modulate gut microbiota to prevent or treat obesity.
The mouse study you was a landmark in microbiome research, demonstrating the causal role of gut microbiota in obesity. While the term “gastric microbiota” refers specifically to the stomach, this study focused on gut microbiota (intestinal microbiota) and its impact on energy harvest and fat storage. Its findings have paved the way for innovative approaches to managing human obesity, including microbiota-based therapies, dietary interventions, and personalized medicine.
The question which is imperative is in people of eastern origins, who eat sushi and curries (India) are there any studies on the microbiota in these communities, to account their low BMIs and an ectomorphic physical type? This question about the microbiota of people from Eastern origins, particularly those who consume diets rich in sushi (Japan) and curries (India), and how their microbial profiles might relate to their generally lower BMIs and ectomorphic (lean) physical types.
- Overview of Eastern Diets and Microbiota
Diets in Eastern cultures, such as Japanese and Indian cuisines, are often rich in specific foods that can shape the gut microbiota in unique ways. These diets are typically high in:
- Fermented foods (e.g., miso, natto, kimchi, yogurt),
- Spices (e.g., turmeric, cumin, ginger),
- Fiber-rich foods (e.g., rice, lentils, vegetables),
- Omega-3 fatty acids (e.g., from fish in sushi).
These dietary components are known to promote a diverse and healthy gut microbiota, which may contribute to lower BMIs and leaner body types.
- Studies on Japanese Microbiota and Sushi Consumption
The Japanese diet, particularly sushi, is rich in fish, seaweed, and fermented foods, which have been shown to influence gut microbiota composition.
- Key Findings
- High Fish Consumption: Fish is a major source of omega-3 fatty acids, which have anti-inflammatory effects and may promote the growth of beneficial bacteria like Lactobacillus and Bifidobacterium.
- Seaweed: Seaweed contains polysaccharides (e.g., alginate) that act as prebiotics, feeding beneficial gut bacteria.
- Fermented Foods: Foods like miso, natto, and soy sauce introduce probiotics (live beneficial bacteria) into the gut, enhancing microbial diversity.
- Microbial Profile
- Studies have shown that Japanese individuals often have a higher abundance of Bacteroidetes, a bacterial phylum associated with leanness, compared to Western populations.
- The Japanese microbiota is also enriched with bacteria capable of breaking down seaweed polysaccharides, such as Bacteroides plebeius.
- Link to Low BMI
- The anti-inflammatory effects of omega-3s and the high fiber content of the Japanese diet may reduce systemic inflammation and improve insulin sensitivity, contributing to lower BMIs.
- The diverse and balanced microbiota promoted by this diet may enhance energy metabolism and reduce fat storage.
- Studies on Indian Microbiota and Curry Consumption
The Indian diet, characterized by its use of spices, lentils, and vegetables[22], also has a significant impact on gut microbiota.
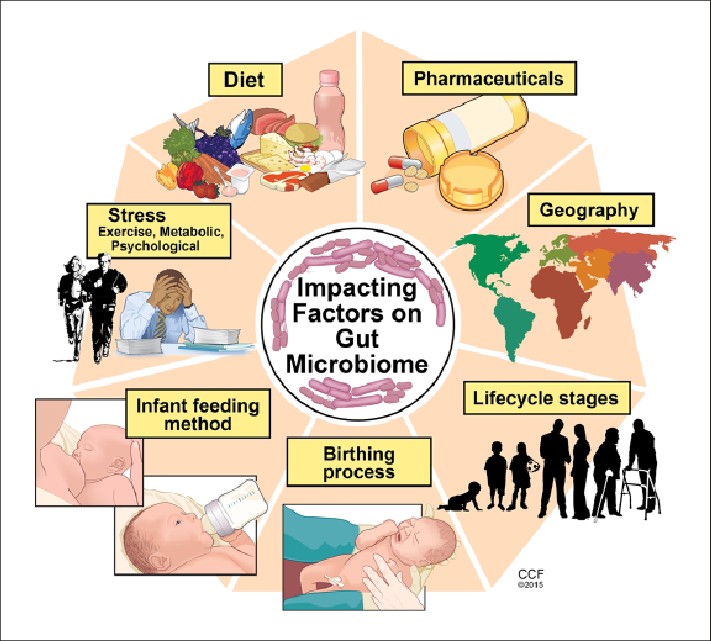
Factors affecting gut microbiome. Illustration by David Schumick, BS, CMI. Reprinted with the permission of the Cleveland Clinic Center for Medical Art & Photography © 2015.
Photo Credit: All rights reserved. CCF, Cleveland Clinic Foundation.
- Key Findings
- Spices:[23] Turmeric, cumin, ginger, and other spices have antimicrobial and anti-inflammatory properties that can shape the gut microbiota.
- Lentils and Legumes: These are rich in fiber and resistant starch, which act as prebiotics and promote the growth of beneficial bacteria.
- Yogurt and Fermented Foods: These introduce probiotics into the gut, enhancing microbial diversity.
- Microbial Profile
- Indian populations often have a higher abundance of Prevotella, a bacterial genus associated with high-fiber diets and leanness.
- The Indian microbiota is also enriched with bacteria capable of metabolizing complex plant polysaccharides.
- Link to Low BMI
- The high fiber content of the Indian diet promotes the production of short-chain fatty acids (SCFAs), which improve metabolic health and reduce fat storage.
- The anti-inflammatory properties of spices may protect against obesity-related inflammation and insulin resistance.
- Comparing Eastern and Western Microbiota
- Western Diets: High in processed foods, sugar, and saturated fats, which promote the growth of Firmicutes (associated with obesity) and reduce microbial diversity.
- Eastern Diets: High in fiber, fermented foods, and spices, which promote the growth of Bacteroidetes and Prevotella (associated with leanness) and enhance microbial diversity.[24]
- Ectomorphic Physical Type and Microbiota[25]
The ectomorphic (lean) body type commonly observed in Eastern populations may be influenced by:
- Microbial Efficiency: A microbiota adapted to high-fiber, plant-based diets may extract fewer calories from food, contributing to leanness.
- Anti-Inflammatory Effects: Diets rich in omega-3s and spices reduce systemic inflammation, which is linked to lower fat accumulation.
- Hormonal Regulation: A healthy gut microbiota can influence hormones like leptin and ghrelin, which regulate appetite and energy balance.
- Challenges and Limitations
- Genetic Factors: Genetics also play a role in body type and metabolism, independent of diet and microbiota.
- Urbanization and Westernization: As Eastern populations adopt more Westernized diets, rates of obesity and related diseases are increasing, highlighting the importance of traditional diets in maintaining a healthy microbiota.
- Individual Variability: Microbiota composition varies widely between individuals, even within the same population.
- Future Research Directions
- Longitudinal Studies: Tracking changes in microbiota and BMI over time in Eastern populations.
- Intervention Studies: Testing the effects of traditional Eastern diets on microbiota and metabolic health in diverse populations.
- Mechanistic Studies: Understanding how specific dietary components (e.g., seaweed polysaccharides, spices) influence microbial pathways and host metabolism.
- Invaluable insights and Lessons Learnt from the Eastern Hemisphere
The traditional diets of Eastern populations, rich in fermented foods, spices, fiber, and omega-3s, promote a diverse and healthy gut microbiota that may contribute to lower BMIs and ectomorphic body types. While genetics and lifestyle also play a role, the microbial profiles of these populations provide valuable insights into the relationship between diet, microbiota, and metabolic health. Preserving these traditional dietary practices could be key to combating the global rise in obesity.
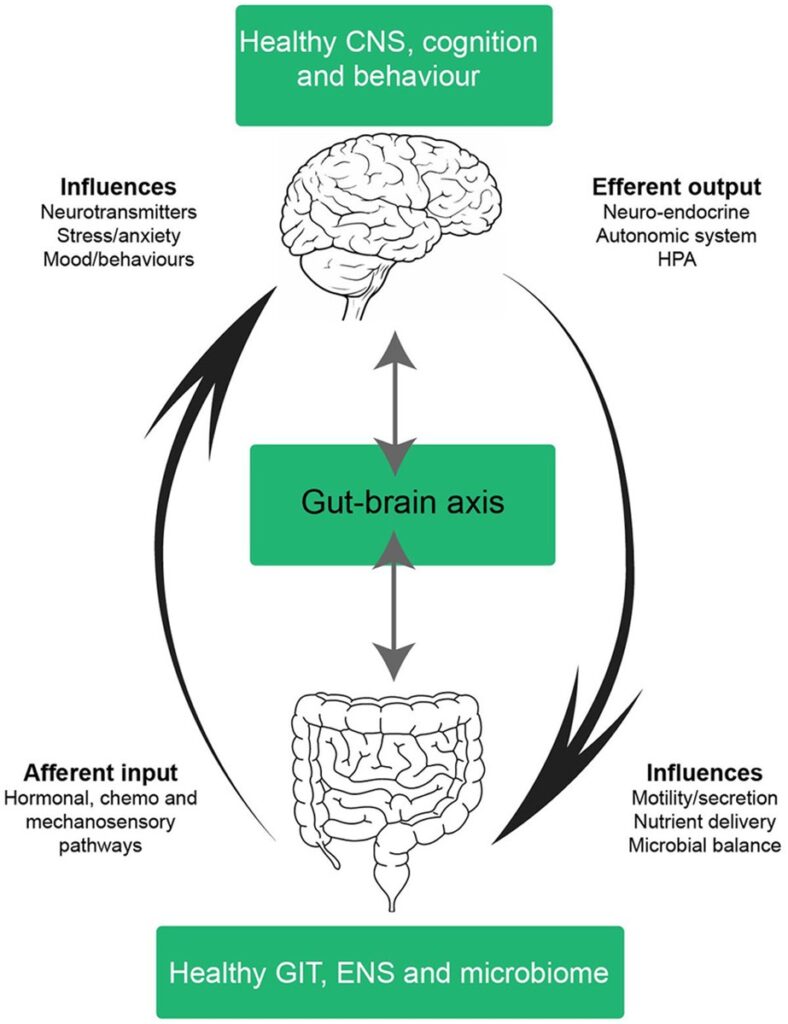
The Gut-Brain Axis [26]
The gastro-intestinal tract talks to the brain and it listens carefully. It then tells the gut what to do to maintain health. This millisecond to millisecond communication is mainly mediated by the Vagus nerve,[27] and is called the GUT-Brain Axis. Abuse of the gut and the brain, by alcohol, drugs, fatty foods and antibiotics results in a dys-coordinated communication, by the Vagus Nerve, resulting in ill health, as the micro-ecosystem of the gut microbiota is disturbed and functionally disrupted, often irreparably. This necessary axis also promotes sugar cravings and preferences. Concentrated research is being undertaken, globally, in the race against the new, ever increasing epidemic of obesity.
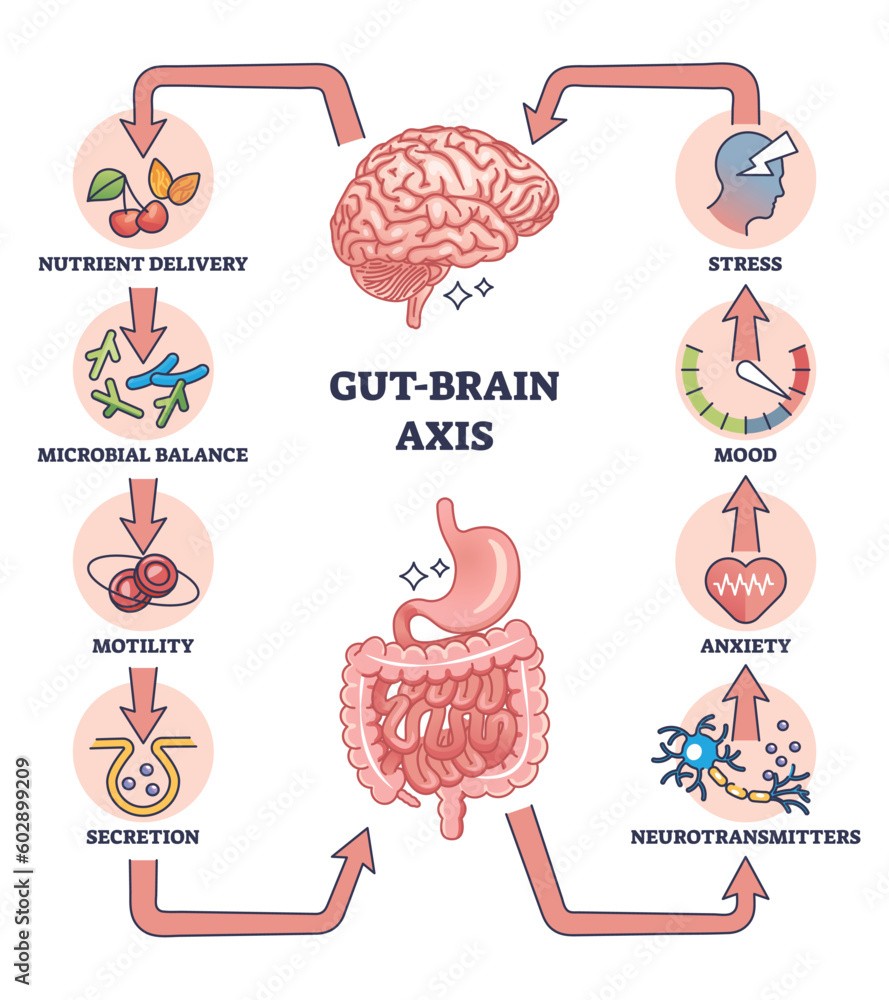
An outline diagram to simplify the Gut-Brain Axis as intestinal and nervous system interaction.
Photo Credit: https://as1.ftcdn.net/jpg/06/02/89/92/1000_F_602899209_AqAHaSDbzMXWHmMTFYNuUrQ9AoCCLvxy.jpg
Schematic of a healthy gut-brain axis. The arrows highlight the bidirectional nature of the gut-brain axis; in a balanced system mechanism from the bottom-up (and vice versa) exist in cohesion. In a healthy system, the gut-brain axis integrates information from many systems; the central nervous system (CNS), autonomic nervous system (ANS), enteric nervous system (ENS), neuroendocrine, enteroendochrine, neuroimmune, and hypothalamic-pituitary axis (HPA). The complex bidirectional communication pathways and systems shared between the gut and the brain maintain health and homeostasis in the CNS, GIT, and microbiota. Efferent signals from the brain involving neuro-endocrine, autonomic and HPA outputs influence motility, secretion, nutrient delivery and microbial balance in the GIT. Whilst afferent inputs from the GIT, such as intestinal hormones, cytokines and sensory perceptions influence neurotransmitter expression, stress, anxiety, mood and behaviour. CNS, central nervous system; ANS, autonomic nervous system; ENS, enteric nervous system; HPA, hypothalamic-pituitary axis; GIT, gastrointestinal tract.
Photo Credit: https://www.researchgate.net/publication/325294793/figure/fig3/AS:11431281153717319@1682523106093/Schematic-of-a-healthy-gut-brain-axis-The-arrows-highlight-the-bidirectional-nature-of.tif
The Bottom Line
The gastric microbiota is a complex and dynamic community that plays a vital role in maintaining gastric health and overall well-being. While H. pylori is the most studied member of this community, other microbes also contribute to its functions. Dysbiosis in the gastric microbiota is linked to various diseases, highlighting the importance of maintaining a balanced microbial ecosystem. Ongoing research holds promise for new diagnostic tools and therapies targeting the gastric microbiota.
The author is of an opinion that a full medical expose on Gastric Microbiota. It is relevant and necessary to elaborate its role in acquired truncal obesity, related to abnormal lifestyle. The relationship between gastric microbiota and acquired truncal obesity (central or abdominal obesity) is an area of growing interest in intense medical research, which if the Big Pharma can find a formula will have the shareholders and directors laughing al the way to the Swiss banking institutions. Truncal obesity, characterized by excessive fat accumulation around the abdomen, is often linked to abnormal lifestyle factors such as poor diet, physical inactivity, stress, and sleep disturbances. Emerging evidence suggests that gastric microbiota, as part of the broader gut microbiome, plays a significant role in the development and progression of obesity, particularly truncal obesity. Below is a detailed exploration of this connection.
References:
[1] https://www.bing.com/ck/a?!&&p=3a02f09d3bd9a900e8f3cea1075086232bd0cbc1a5379f7f5caf917a5a5ecafbJmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=The+Human+Microbiome%3a+A+new+frontier+in+health+&u=a1aHR0cHM6Ly93d3cubmF0dXJlLmNvbS9hcnRpY2xlcy9zNDEzOTItMDI0LTAxOTQ2LTY&ntb=1
[2] https://www.walshmedicalmedia.com/open-access/the-impact-of-microbiome-on-human-health-a-new-frontier-in-disease-prevention-and-treatment.pdf
[3] https://www.ck12.org/book/ck-12-biology/section/17.2/
[4] Ruppert EE, Fox RS, Barnes RD (2004). “Introduction to Bilateria”. Invertebrate Zoology (7 ed.). Brooks / Cole. p. 197 [1]. ISBN 978-0-03-025982-1
[5] https://web.archive.org/web/20090628224336/http://www.mercksource.com/pp/us/cns/cns_hl_dorlands_split.jsp?pg=/ppdocs/us/common/dorlands/dorland/eight/000109945.htm
[6] https://meshb.nlm.nih.gov/record/ui?name=Gastrointestinal+tract
[7] https://web.archive.org/web/20090628224336/http://www.mercksource.com/pp/us/cns/cns_hl_dorlands_split.jsp?pg=/ppdocs/us/common/dorlands/dorland/nine/000952042.htm
[8] https://en.wikipedia.org/wiki/Gastrointestinal_tract#:~:text=G.%2C%20Hounnou%3B%20C.%2C%20Destrieux%3B%20J.%2C%20Desm%C3%A9%3B%20P.%2C%20Bertrand%3B%20S.%2C%20Velut%20(2002%2D12%2D01).%20%22Anatomical%20study%20of%20the%20length%20of%20the%20human%20intestine%22.%20Surgical%20and%20Radiologic%20Anatomy.%2024%20(5)%3A%20290%E2%80%93294.%20doi%3A10.1007/s00276%2D002%2D0057%2Dy.%20ISSN%C2%A00930%2D1038.%20PMID%C2%A012497219.%20S2CID%C2%A033366428
[9] https://www.bing.com/ck/a?!&&p=1e774cb5fd5944bb28eee403613888c5cf1d53c4277ba9f0b5c9002ee2c7c175JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=Role+of+Helicobacter+pylori+on+microbiome&u=a1aHR0cHM6Ly9qb3VybmFscy5wbG9zLm9yZy9wbG9zb25lL2FydGljbGU_aWQ9MTAuMTM3MS9qb3VybmFsLnBvbmUuMDIxODI3NCM6fjp0ZXh0PUhlbGljb2JhY3RlciUyMHB5bG9yaSUyMCUyOEguJTIwcHlsb3JpJTI5JTIwaXMlMjBrbm93biUyMHRvJTIwY29sb25pemUsYmVlbiUyMGxpbmtlZCUyMHdpdGglMjB2YXJpb3VzJTIwbWV0YWJvbGljJTIwYW5kJTIwaW5mbGFtbWF0b3J5JTIwZGlzZWFzZXMu&ntb=1
[10] https://www.bing.com/ck/a?!&&p=61030d1c40bab7734d1b060309f5560ee1c224dc446c0301730c2fe6ac46edf1JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=Sleep+Disturbances+and+microbiome&u=a1aHR0cHM6Ly93d3cuc2NpZW5jZWRpcmVjdC5jb20vc2NpZW5jZS9hcnRpY2xlL3BpaS9TMTM4OTk0NTcyMTAwNDM1NA&ntb=1
[11] https://www.bing.com/ck/a?!&&p=6c113eb71b0ee89be05d67ef75f7a7b3b289589f7631b62d3d909937e82a3f4cJmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=Sleep+Disturbances+and+microbiome&u=a1aHR0cHM6Ly9wbWMubmNiaS5ubG0ubmloLmdvdi9hcnRpY2xlcy9QTUM2MjkwNzIxLw&ntb=1
[12] https://www.bing.com/ck/a?!&&p=cfd82f781082df6abc42b65256bb83316833033b7370429fc1011deb90d4d82eJmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=Alcohol+and+Smoking+Excessive+alcohol++on+microbiome&u=a1aHR0cHM6Ly93d3cuc2NpZW5jZWRpcmVjdC5jb20vc2NpZW5jZS9hcnRpY2xlL3BpaS9TMjIxNDc5OTMyMDMwMDc4Mw&ntb=1
[13] https://www.bing.com/ck/a?!&&p=1cfd23dd7f9bdc2ec1ed046a86a9e92abe692a64d49171bc3fd78af94e71fc62JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=.+Clinical+Evidence+Linking+Gastric+Microbiota+to+Truncal+Obesity&u=a1aHR0cHM6Ly93d3cubmNiaS5ubG0ubmloLmdvdi9wbWMvYXJ0aWNsZXMvUE1DOTIyOTc4NS8&ntb=1
[14] https://www.bing.com/ck/a?!&&p=1cfd23dd7f9bdc2ec1ed046a86a9e92abe692a64d49171bc3fd78af94e71fc62JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=.+Clinical+Evidence+Linking+Gastric+Microbiota+to+Truncal+Obesity&u=a1aHR0cHM6Ly93d3cubmNiaS5ubG0ubmloLmdvdi9wbWMvYXJ0aWNsZXMvUE1DOTIyOTc4NS8&ntb=1
[15] https://www.bing.com/ck/a?!&&p=c04710e8438b3324c86f150ab21ccf57b5be285034571c95848c641b42ca17e5JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=%e2%80%a2%09higher+levels+of+Firmicutes+and+lower+levels+of+Bacteroidetes.&u=a1aHR0cHM6Ly93d3cucnVwYWhlYWx0aC5jb20vcG9zdC90aGUtZmlybWljdXRlcy1iYWN0ZXJvaWRldGVzLXJhdGlvLXdoYXQtaXQtbWVhbnMtZm9yLWd1dC1oZWFsdGgtaG9ybW9uZXMtYW5kLW92ZXJhbGwtd2VsbG5lc3M&ntb=1
[16] https://www.bing.com/ck/a?!&&p=08d2cca557a338e9092ca086e850a35e7988a3c3f2a0bdcd5b7f480a753f5931JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=%e2%80%a2%09higher+levels+of+Firmicutes+and+lower+levels+of+Bacteroidetes.&u=a1aHR0cHM6Ly9iaW9wdGltaXplcnMuY29tL2Jsb2cvd2hhdC1hcmUtYmFjdGVyb2lkZXRlcy1maXJtaWN1dGVzLz9nbD02Mzg4MDQwMTNmNWQ2MGI0MDE4YjQ1Njg&ntb=1
[17] https://www.bing.com/ck/a?!&&p=dfc73eb6ef3e943b32235d0e4855c3d89e4f34bf8a85ea680468d86436cb2dfeJmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=faecal+microbiota+transplantation+fmt&u=a1aHR0cHM6Ly9lbi53aWtpcGVkaWEub3JnL3dpa2kvRmVjYWxfbWljcm9iaW90YV90cmFuc3BsYW50&ntb=1
[18] https://www.bing.com/ck/a?!&&p=1e4c132dd0d7e60c52b923365e2326a96f76fc64faaa8a59f4707361cac1d3e4JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=Personalized+Nutrition&u=a1aHR0cHM6Ly9wbWMubmNiaS5ubG0ubmloLmdvdi9hcnRpY2xlcy9QTUMxMTM1NzQxMi8&ntb=1
[19] https://www.bing.com/ck/a?!&&p=b718f4cb69d48067373277b28f56a5b0fa45bb5b7b52ba48cb5dd5937fb178b6JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=Microbiome-Based+Biomarkers&u=a1aHR0cHM6Ly93d3cubWljcm9iaW9tZXRpbWVzLmNvbS9taWNyb2Jpb21lLWJhc2VkLWRpYWdub3N0aWNzLWFuZC1iaW9tYXJrZXJzLWNoYW5naW5nLXRoZS1wYXJhZGlnbS1pbi1taWNyb2Jpb2xvZ3ktYW5kLW1lZGljaW5lLyM6fjp0ZXh0PU1pY3JvYmlvbWUtYmFzZWQlMjBkaWFnbm9zdGljcyUyMGFyZSUyMHRvb2xzJTIwdGhhdCUyMGFsbG93JTIwZGV0ZWN0aW9uJTIwb2YlMkMsYSUyMGJvZHklMjBzaXRlJTIwZGlzdGFudCUyMGZyb20lMjB0aGUlMjBkaXNlYXNlJTIwc2l0ZS4&ntb=1
[20] https://www.bing.com/ck/a?!&&p=a45e4f57ca833443c3b46dec83a8038ba7663dcae32c351c059631516ea7a056JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=microbiome+and+degerative+brain+diseases&u=a1aHR0cHM6Ly9saW5rLnNwcmluZ2VyLmNvbS9hcnRpY2xlLzEwLjEwMDcvczExMDEwLTAyMy0wNDg1My02&ntb=1
[21] https://www.bing.com/ck/a?!&&p=f664eae315e1519111bb34c72fcd6260e5ab2aed1133cab0eebd61c4ac2baa55JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=microbiome+and+degerative+brain+diseases&u=a1aHR0cHM6Ly9wbWMubmNiaS5ubG0ubmloLmdvdi9hcnRpY2xlcy9QTUM5MTgyMDAyLw&ntb=1
[22] https://www.bing.com/ck/a?!&&p=b91fe9f3c4938d6d846e3697e87d2b39b7d825f90092a46820052f88a63f4d73JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=vegetarian+diet+benefits+on+gut+microbiome&u=a1aHR0cHM6Ly9wbWMubmNiaS5ubG0ubmloLmdvdi9hcnRpY2xlcy9QTUM2NDc4NjY0Lw&ntb=1
[23] https://www.bing.com/ck/a?!&&p=5a2e8ab9e337b3dd985a613e2c50ea272c14cd8aea04bf25ba0b1ba83eb148d0JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=best+spices+for+microbiome&u=a1aHR0cHM6Ly93d3cudXNlbm91cmlzaC5jb20vYmxvZy9oZXJicy1mb3ItZ3V0LWhlYWx0aA&ntb=1
[24] https://www.bing.com/ck/a?!&&p=df79633ef519975a0cb01d02559101824fd27d28e876e82eb22763c4cd80e50fJmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=%e2%80%a2%09Bacteroidetes+and+Prevotella+(associated+with+leanness)+and+enhance+microbial+diversity.&u=a1aHR0cHM6Ly9taWNyb2Jpb21lam91cm5hbC5iaW9tZWRjZW50cmFsLmNvbS9hcnRpY2xlcy8xMC4xMTg2L3M0MDE2OC0wMTYtMDE2MC03&ntb=1
[25] https://www.bing.com/ck/a?!&&p=75da61296377754dca69f28db7f348a320ea94a27275165af0e1c1ef3d0c8da2JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&u=a1L2ltYWdlcy9zZWFyY2g_cT0xLitlY3RvbW9ycGhpYytwaHlzaWNhbCt0eXBlK2FuZCttaWNyb2Jpb3RhJnFwdnQ9MS4lMDlFY3RvbW9ycGhpYytQaHlzaWNhbCtUeXBlK2FuZCtNaWNyb2Jpb3RhJkZPUk09SUdSRQ&ntb=1
[26] https://www.bing.com/aclick?ld=e8kTIeWXtO7Gpo2NDzTZ1mXDVUCUxZZ6NqrnM3cXBvjWuV-lZqAof0nu64Mxsjk88hp_Fi0Y1Y5-KPD6Kj0AW2ewcJcP3u7ZnkIyiGyJM0IAMt-GUCghGvpJIG59Ycn6n3FqZ6n2eQ0OQmDBD4rnrUY3uN4uKZ_hkQl5Rni-nix7uYTp5UcjfxOr4uR8pR28SPw5dmig&u=aHR0cHMlM2ElMmYlMmZ3d3cudWRlbXkuY29tJTJmY291cnNlJTJmZ3V0LWJyYWluLWF4aXMtdW5jb3ZlcmVkJTJmJTNmdXRtX3NvdXJjZSUzZGJpbmclMjZ1dG1fbWVkaXVtJTNkdWRlbXlhZHMlMjZ1dG1fY2FtcGFpZ24lM2RCRy1TZWFyY2hfRFNBX0dhbW1hQ2F0Y2hhbGxfTm9uUF9sYS5FTl9jYy5ST1ctRW5nbGlzaCUyNmNhbXBhaWdudHlwZSUzZFNlYXJjaCUyNnBvcnRmb2xpbyUzZEJpbmctUk9XLUVuZ2xpc2glMjZsYW5ndWFnZSUzZEVOJTI2cHJvZHVjdCUzZENvdXJzZSUyNnRlc3QlM2QlMjZhdWRpZW5jZSUzZERTQSUyNnRvcGljJTNkJTI2cHJpb3JpdHklM2RHYW1tYSUyNnV0bV9jb250ZW50JTNkZGVhbDQ1ODQlMjZ1dG1fdGVybSUzZF8uX2FnXzEzMjE2MTUzNjUwNDE2NDBfLl9hZF9fLl9rd191ZGVteV8uX2RlX2NfLl9kbV9fLl9wbF9fLl90aV9kYXQtMjMzNDQwMDYyNTM5MTQyOSUzYWxvYy0xNjhfLl9saV8xMzc4MTJfLl9wZF9fLl8lMjZtYXRjaHR5cGUlM2RiJTI2bXNjbGtpZCUzZGE5NmY0YjJhNzJjZDEwMzExYjA2MmNmZjhiYzIyNTkw&rlid=a96f4b2a72cd10311b062cff8bc22590&ntb=1
[27] https://www.bing.com/ck/a?!&&p=7a84f49cbcd3c733ff551e2a28828eefde36ef33f2ba5b6dc65f26b830e25f07JmltdHM9MTc0MTk5NjgwMA&ptn=3&ver=2&hsh=4&fclid=19bf7366-9926-65b9-0269-601d982664b6&psq=vagus+nerve+exercises&u=a1aHR0cHM6Ly9oZWFsdGguY2xldmVsYW5kY2xpbmljLm9yZy92YWd1cy1uZXJ2ZS1zdGltdWxhdGlvbg&ntb=1
______________________________________________
 Professor G. Hoosen M. Vawda (Bsc; MBChB; PhD.Wits) is a member of the TRANSCEND Network for Peace Development Environment.
Professor G. Hoosen M. Vawda (Bsc; MBChB; PhD.Wits) is a member of the TRANSCEND Network for Peace Development Environment.
Director: Glastonbury Medical Research Centre; Community Health and Indigent Programme Services; Body Donor Foundation SA.
Principal Investigator: Multinational Clinical Trials
Consultant: Medical and General Research Ethics; Internal Medicine and Clinical Psychiatry:UKZN, Nelson R. Mandela School of Medicine
Executive Member: Inter Religious Council KZN SA
Public Liaison: Medical Misadventures
Activism: Justice for All
Email: vawda@ukzn.ac.za
Tags: Health
This article originally appeared on Transcend Media Service (TMS) on 17 Mar 2025.
Anticopyright: Editorials and articles originated on TMS may be freely reprinted, disseminated, translated and used as background material, provided an acknowledgement and link to the source, TMS: Endogenous Pursuit of Peace: Care about Your Microbiota, is included. Thank you.
If you enjoyed this article, please donate to TMS to join the growing list of TMS Supporters.

This work is licensed under a CC BY-NC 4.0 License.
Join the discussion!
We welcome debate and dissent, but personal — ad hominem — attacks (on authors, other users or any individual), abuse and defamatory language will not be tolerated. Nor will we tolerate attempts to deliberately disrupt discussions. We aim to maintain an inviting space to focus on intelligent interactions and debates.